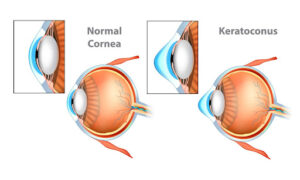
Keratoconus is an uncommon condition that causes a progressive thinning and bulging of the cornea, the clear front portion of the eye that focuses light into your eye helping you to see clearly. As this condition progresses, the cornea develops a cone-like bulge. This conic shape changes the way the cornea focuses the light, distorting and blurring vision.
Approximately 1 in 2,000 people are affected by keratoconus, and for most part, it manifests in their teen years, progressively worsening until it stabilizes in their 30s and 40s. It usually affects both eyes, however the progression and symptoms may differ in each eye, causing drastically different vision between them. Though vision may become significantly impaired, causing difficulty with simple tasks and driving, blindness is rarely a result.
What causes keratoconus?
Though we aren’t sure of the cause, some researchers suspect there may be a genetic link since an estimated 10% of patients with keratoconus have a family member with the disease.
Some other things that could be associated with Keratoconus are:
- Eye allergies
- Excessive eye rubbing
- Connective tissue disorders like Marfan syndrome and Ehlers-Danlos syndrome
according to the American Academy of Ophthalmology.
What are the symptoms of keratoconus?
As stated, though keratoconus typically affects both eyes, it often causes very different vision in each.
Early symptoms include:
- Sensitivity to light
- Mild blurring
- Distortion of vision (do straight lines look wavy?)
- Eye redness or swelling
Later symptoms:
- Increase in blurry and distorted vision
- Increase in nearsightedness and/or astigmatism (do you often need new eyeglass prescriptions?)
- Inability to wear contact lenses because of fit or discomfort
These symptoms can take many years to progress. However, for some, the cornea can swell and scar quite suddenly. It is important to address any symptoms you may have as quickly as possible by making an appointment at your local eye center.
How is keratoconus diagnosed?
After you’ve called your eye doctor’s office, you’ll be scheduled for a routine eye exam. During your exam, your doctor will review your medical and family history. Then, your cornea will be observed and its curvature may be measured if a change in shape is detected. The Mayo Clinic informs, tests for keratoconus include:
- Eye refraction- An evaluation of your eyes with a phoropter or retinoscope
- Slit-lamp examination- Shining a light on the surface of your eye to look at the shape of your cornea
- Keratometry- Measuring the reflection of light on your cornea
- Computerized corneal mapping- Using corneal tomography and topography to create a shape map of your cornea and measure its thickness
What treatments are available for keratoconus?
There are several treatments for keratoconus depending on your symptoms and the severity of the disease.
Eyeglasses
Generally, when symptoms are mild, eyeglasses are used to correct vision in keratoconic patients.
Scleral contact lens (a specially designed kind of rigid gas permeable contact lens (RGP)
If the symptoms worsen, or if you are a contact wearer, a specialized, rigid gas permeable contact lens, called a scleral lens, can be used to achieve focused vision. This specific RGP is contoured to address the cone-like shape of the cornea thereby improving vision. A proper fitting lens is vital in providing a comfortable fit and adequate vision, and typically requires an eye care provider who is experienced with this kind of lens as it is not a standard RGP lens.
Intacs®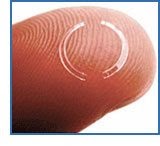
When contacts and glasses can no longer provide adequate vision, Intacs® corneal implants provide a much less invasive treatment option. The small, crescent-shaped, acrylic device is surgically placed in the mid-periphery of the cornea in an effort to flatten the curvature. They have been shown to be effective, improving vision and postponing a corneal transplant in many patients.
Benefits of Intacs® for Keratoconus
- Safe, replaceable, removable
- Decreases nearsightedness and astigmatism associated with keratoconus
- A more natural dome shape is restored to the cornea
- A few days of recovery compared to months for a corneal transplant
- May postpone the need for a corneal transplant
Corneal cross-linking
An additional option is called corneal cross-linking, which is the only treatment that can stop progressive keratoconus from getting worse. In this procedure, doctors use eyedrop medication and ultraviolet (UV) light from a special machine to make the tissues in your cornea stronger. The goal is to “flatten or stiffen your cornea, keeping it from bulging more.”
It’s called “cross-linking” because it adds bonds between the collagen fibers in your eye. They work like support beams to help the cornea stay stable. This procedure may help to avoid a corneal transplant.
Corneal transplant
Though it is a last resort, if keratoconus is advanced or the eye has scars in the visual axis, corneal transplantation may still be the best answer. Your ophthalmologist would perform a surgical procedure to replace all or part of your cornea with donor tissue. “Most cornea transplant procedures are successful,” the Mayo Clinic assures. “But cornea transplant carries a small risk of complications, such as rejection of the donor cornea.”
What to remember about keratoconus
If you have:
- Sensitivity to light
- Blurry or distorted vision
- Eye redness or swelling
Call your Boulder, Longmont, Lafayette, or Greeley eye center for an eye exam immediately.
And don’t rub your eyes. Rubbing the eyes can further damage your corneal tissue. Ask your eye doctor about other ways to treat itchy eyes.
Schedule your next eye exam with the Eye Care Center of Northern Colorado today! We’ve built our entire practice around getting you the best and most comprehensive care.
Check out our Patient Education Portal for more information or peruse these related blogs for more keratoconus and eye health facts:
References and Resources
https://eyecaresite.com/multispecialty-eye-surgery/cornea/keratoconus-treatment/
https://eyecaresite.com/cornea-and-refractive-specialist/common-corneal-disorders/
https://www.aao.org/eye-health/diseases/keratoconus-cause
https://www.aao.org/eye-health/diseases/keratoconus-symptoms
https://www.mayoclinic.org/diseases-conditions/keratoconus/diagnosis-treatment/drc-20351357
https://eyecaresite.com/multispecialty-eye-surgery/cornea/cornea-transplants/
https://eyecaresite.com/multispecialty-eye-surgery/cataract/keratoconus-intacs/
https://www.aao.org/eye-health/diseases/keratoconus-diagnosis
https://www.mayoclinic.org/tests-procedures/cornea-transplant/about/pac-20385285